Trigger Warning: This blog mentions suicide.
At the start of the day a canary is singing, ruffling its wings, head up high. It is then taken deep underground with all the miners. At the end of the day when they all return to the surface, the canary is covered in black coal dust, probably coughing, head bowed. No one would say, “Why did the canary make itself sick?” because they know that it was the work environment that made the canary ill.
I heard this analogy (originally from Christina Maslach, Professor of the Graduate School, UC Berkeley Psychology), during an excellent workshop run by my colleague Stephen Haynes, Director of Wellbeing, British Safety Council and it stuck with me
It would never cross our minds that the canary had purposefully made itself ill through doing its job, so why don’t we pay more attention to how our work environments can affect the mental health of employees?
If we continue with the canary analogy, being diligent employers, the mine supervisors/managers would look at the canary, identify what was making it sick and make reasonable work adjustments, so its physical health did not continue to deteriorate. For the canary, that might be an improvement to its cage so it could still detect the dangerous gases but be protected from the dust.
Whilst many businesses are geared to identifying and mitigating physical risks, why do only a small percentage do the same for mental health risks? This is despite the fact that, ‘employers have a legal duty to protect workers from stress at work by doing a risk assessment and acting on it. This is the same duty you have to protect people from other health and safety risks’ (Health and Safety Executive). Worryingly, our survey found that fewer than 10% of respondents said that their “line managers know how to undertake stress risk assessments and understand when they may be necessary” (almost 70% said they would not).
Therefore, in this blog we will be addressing the following questions:
- Why don’t we notice when someone experiences mental ill-health due to their work?
- What is causing this situation?
- What can we do to stop it?
Building Positive Mental Health in the Workplace
With World Mental Health Day (10 October), Men’s Health Awareness Month (November) and National Stress Awareness Day (5 November), it has never been more vital that we dedicate time to learn what we, as employers, colleagues and community members, can do to build positive mental health in and through work.
We have created a suite of resources which are designed to provide organisations with information, tools and templates to build proactive cultures of prevention.
Supporters, please log in to download your exclusive resources from the portal.
What are the statistics on mental health?
- 776,000 workers experienced work-related stress, depression or anxiety in 2023/24.
- Stress, depression or anxiety accounted for 46% of work-related ill health and 55% of all working days lost due to ill health in 2023/24.
- In 2023, there were 7,055 deaths in the UK officially registered as suicide.
In the higher-risk sectors in which we work:
- Construction:
- The 2025 CIOB report found that:
- 58% of respondents experienced stress, 50% experienced anxiety and 21% experienced depression ‘often’ i.e., daily or weekly.
- 27% of construction workers had experienced thoughts of suicide at some point in the previous year (up from 26% in 2020).
- 58% of respondents experienced stress, 50% experienced anxiety and 21% experienced depression ‘often’ i.e., daily or weekly.
- In 2021, 507 construction workers died by suicide. (ONS and Glasgow Caledonian University)
- The 2025 CIOB report found that:
- Transport and logistics:
- Randstad’s 2023 ‘Health and Well-being in the Workplace’ report found that 27% of logistics workers surveyed had taken time off work due to unmanageable stress or mental health conditions in the previous 12 months, and 19% of respondents were planning to leave the profession in the next 12 months because of it.
- In 2017 the Office for National Statistics reported that drivers of forklift trucks had a suicide rate 85% higher than the national average. Van drivers were noted to have a rate 25% higher, and drivers of large goods vehicles 20% higher than the national average.
- Randstad’s 2023 ‘Health and Well-being in the Workplace’ report found that 27% of logistics workers surveyed had taken time off work due to unmanageable stress or mental health conditions in the previous 12 months, and 19% of respondents were planning to leave the profession in the next 12 months because of it.
- Farming and agriculture:
- 91% of farmers and agricultural workers agreed that poor mental health is the 'biggest hidden problem' facing the industry today.
- Office of National Statistics figures showed 44 suicides were registered in England & Wales among the farming and agricultural industry in 2022.
- 91% of farmers and agricultural workers agreed that poor mental health is the 'biggest hidden problem' facing the industry today.
Why Don’t We Notice When Someone Is Experiencing Mental Ill-Health?
If you notice a physical change in someone, for example, they are coughing and sneezing, have a plaster cast on their leg, or are wearing a glucose monitor on their arm, you would know they had a physical ailment or disability, and would ask if they are ok and discuss what support you can provide. But would you notice if someone was experiencing mental ill-health or a mental illness? If you did notice, would you feel uncomfortable and more likely to overlook them, because it was a mental rather than physical condition?
It is all too easy to miss what is going on around us when we are experiencing a heavy workload or under pressure to meet a deadline. This could result in us missing a formal catch up during a one-to-one or team meeting, or an informal chat during a lunch break. But, as we saw above, if you are a line manager, you have a duty to undertake individual stress risk assessments and act on them, i.e., to make reasonable work adjustments (if required) and provide ongoing support to the team member.
This means that if you are in a position with managerial responsibilities, it is essential to keep up those regular check-ins with everyone in your team. This is important because stress doesn’t sit in isolation - it shapes how people think, feel, behave, and perform at work. Therefore, in addition to being a legal and moral duty, it is also a core business issue, because it drives engagement, turnover, innovation, creativity, and collaboration.
How Do You Know When an Individual Stress Risk Assessment Is Needed?
In an ideal world, the answer to that is simple. Create a workplace culture where understanding, identifying and mitigating stress is at its very core. A culture where there is no stigma around mental health, and conversations about it are normalised and encouraged. This will help to reduce the likelihood of workplace mental ill-health and, importantly, give your employees the confidence to come to you if/when they are experiencing it. This last point is significant, because a 2024 survey by Aviva, found that fewer than 6% of men and 4% of women said they would discuss their mental health experiences with their employer. In fact, 33% of men said they would never discuss mental health in the workplace.
However, in the real world, it is more likely that individual stress risk assessments will be conducted when a staff member reports work-related stress, is on sick leave because of it, or is returning to work after an absence caused by it.
In addition, building a culture of prevention does not happen overnight, so it is important to know how to spot the signs.
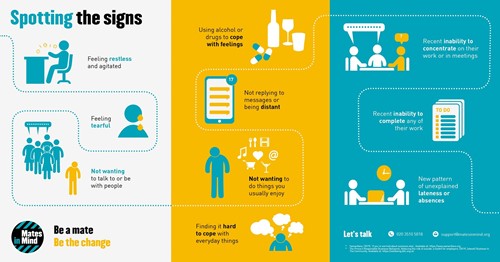
The infographic below shows some of the signs that someone might be experiencing stress, anxiety or depression, but it is important to remember that we are all different and some people can mask how they are feeling. The answer is to be observant, notice when someone is behaving ‘out of character’ for them and take action. Changes could include work standards slipping, being late for work, drinking more heavily, not talking or wanting to be with people, being more irritable etc. You can download the infographic from our Resources page.
The other issue is that people do not always feel confident to start a conversation – due to worrying that they may say or do the wrong thing or offend someone by suggesting they may not be themselves. These are all myths. You do not need to have all the answers, just listening to someone talk about how they are feeling and signposting to further support, can save a life.
Recent research from MHFA England, found that ‘More than half (52%) of respondents said they lacked the confidence or skills to ask someone directly about suicide. Over 43% said they would be worried about how the person might react, and nearly 29% feared that asking might, “put the idea in their head”’. Again, the last of these is a myth, and this is where training comes in, as it provides employees with the skills, knowledge and confidence to start conversations.
Find out about our training courses which include ‘Start the Conversation’ (for all employees), ‘Manage the Conversation’ (for line managers and supervisors), and Mental Health First Aid (for everyone).
What Can Cause Work-Related Mental Ill-Health?
Obviously the causes, and how they impact on someone, vary by sector, organisation, the individual and their line manager. However, it can include long and irregular hours; working away from home; tight deadlines; late payments and economic insecurity; lone working, isolation and lack of support; intense physical work (e.g., construction, farming) or lack of it; working outside in all weather conditions etc,. can impact on our mental and physical health.
Our survey of SME and sole traders working in the construction sector found that:
- I worry that my workload is too high (42% experiencing this frequently).
- I feel low because of my business partners/colleagues (37%).
- I feel low because of pressure at work (35%).
- I feel anxious about family or relationship problems (33%).
- I feel stressed by financial problems or debt (32%).
- Other concerns included impact that work has on family life and worries about being hurt or injured at work.
- Demands - workload and how challenging it is.
- Control - how much control there is over how, when and where work is done.
- Support - how much help is provided to do the job (when required) and how much training is provided.
- Role - whether the job is right, whether someone wants to do it, and if they can do it.
- Relationships - how people get on with their colleagues, including their line manager, and how well everyone works together.
- Change - how much notice is given about upcoming changes and whether or not everyone agrees with them.
It also comes down to whether your line managers are inhibitors (i.e., they simply manage and/or create stress) or enablers (i.e., they help your team to thrive in the workplace through leading, inspiring and coaching).
How Can Companies Improve Mental Health in the Workplace?
Let’s start by looking at the types of intervention you may currently be employing:
- Primary: this is about organisation wide prevention, i.e., identifying and mitigating risk, e.g., organisational culture, policies, management etc., as well as identifying and filling gaps in provision.
- Secondary: this is about prevention at an employee level, e.g., upskilling individuals.
- Tertiary: is treatment, i.e., providing solutions at the point of need, e.g., Employee Assistance Programmes (EAPs) and helplines.
All three stages are important, necessary and need to be optimised. However, at Mates in Mind we advocate for a focus on prevention, i.e., proactive interventions (primary and secondary) in order to provide support before someone reaches the point of crisis.
It is important to remember the analogy at the start of this blog. The canary did not make itself sick, and neither do employees. We cannot train people not to get stressed, or to experience burnout, but we can look at the extent to which factors (detailed in the previous section) impact the mental wellbeing of our teams.
If you treat mental health as a tick box exercise, which focuses on solutions through one-off talks, yoga classes and an Employee Assistance Programme that no one is aware of, rather than stopping and looking at the root causes, then you will not build a culture of prevention. However, if you want to create a culture where stress factors are identified and mitigated, where people openly talk about mental health and seek support when they need it, then you need to:
- Start by getting management buy in (along with their support and leadership).
- Ensure you continually assess where you are on your mental health journey and fill any gaps you identify.
- Equip leaders, managers and HR to identify and mitigate the factors negatively impacting on mental health.
- Ensure all employees have an understanding of psychological first aid.
- Create internal peer networks.
Please read our blog ‘How to optimise mental wellbeing through workplace culture’ for more details on these steps.
Solutions
In addition to downloading the World Mental Health Day resources, please also visit our information and resources page to download infographics, guides and factsheets on stress, spotting the signs of mental ill-health, supporting someone experiencing anxiety, and more. There are also five short stress awareness videos and a mental health quiz to watch.
Ensure you have plans in place to train all of your staff, so that you can build a mentally resilient team. Our suite of mental health and wellbeing training courses are designed for employees at all levels of your organisation, on how to support someone who is experiencing mental ill-health.
Read our other blogs in the series which include creating a supportive workplace culture, eradicating the stigma that surrounds mental health, optimising the mental wellbeing of those around you, and much more:
Finally, speak to us about how we can help you to create a culture of prevention – starting with a comprehensive assessment of where you are on the mental health journey, a tailored plan for how to fill the gaps in your provision, a free course and peer support webinars, access to exclusive resources and templates, as well as a dedicated Support Manager to guide you on your journey. Find out more about how you can become a supporter today.
Further Reading
The following articles provide more insight to support the guidance above. You can learn more about suicide prevention and postvention, explore how workplace culture influences mental wellbeing, and find advice on eradicating the culture of silence and addressing the stigma. For practical, step-by-step guidance, see How to support others to optimise their mental wellbeing – part 1 and part 2.
Conclusion
If this blog has resonated with you, please remember you are not alone. Reach out to a colleague, family member, your GP, call NHS 111, or the Samaritans on 116 123. You can also find further support through our support services page.
If you value our blogs and want to get involved, there are lots of ways to do so. You could join our community, make a donation, or request a call back. You can also share this blog on your socials and tag us, or sign up to our newsletter to stay updated.
Remember, you are not alone — there is always someone to talk to or somewhere to find additional help.